Retinal vein occlusion
MetWest is able to offer patients prompt and up-to-date management for RVO including laser and intravitreal therapy.
The management of RVO is mainly the identification and management of the risk factors, and treating the complications such as macular swelling (oedema). The decision to actively treat macula oedema depends on the patient’s vision, amount of oedema and vision in the other eye. Treatment options eye injections and laser. In clinical trials, on average, patient gained an increase of 11 – 17 letters from presentation with eye injections.
It is important that patients understand that it is often a “course” of injections to manage the macular oedema, with multiple or ongoing injections several weeks apart.
What is retinal vein occlusion?
Retinal vein occlusions (RVO) are the second most common retinal vascular disorder after diabetic retinopathy, and are an important cause of visual loss. The occlusion (blockage) can occur in one of several different veins, and are referred to as “branch”, “central” or “hemi” retinal vein occlusions.
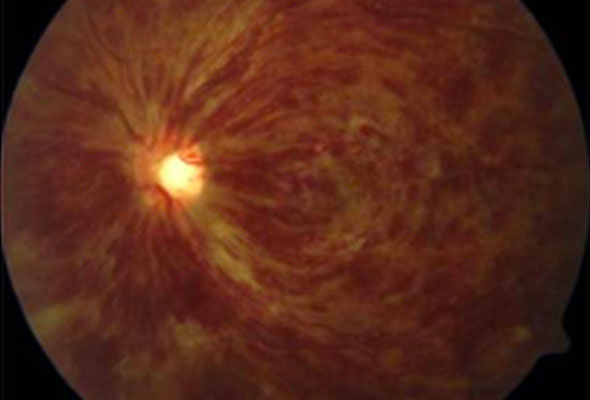
Retinal vein occlusion occurs when the blood vessels supplying the eye are blocked.
Who is at risk of retinal vein occlusion?
RVOs most commonly occur in people in their 50’s and 60’s and affect both genders equally. Risk factors for RVOs include increased age, hypertension, cardiovascular disease, high BMI, hyperlipidaemia and smoking. High intraocular pressure (glaucoma) is an additional risk factor for CRVOs.
What are the symptoms of retinal vein occlusion?
People typically notice a painless decrease in vision or may notice the part of their vision is greyed out / missing. Symptoms of RVO can vary widely from a spectacular sudden loss of vision involving central vision, to not noticing anything at all and the occlusion being detected at an eye examination.
How is a retinal vein occlusion assessed?
The diagnosis of RVO is usually made with testing including fluorescein angiography (FFA) and optical coherence tomography (OCT). OCT is important for detecting macula swelling and monitoring the response to treatment.
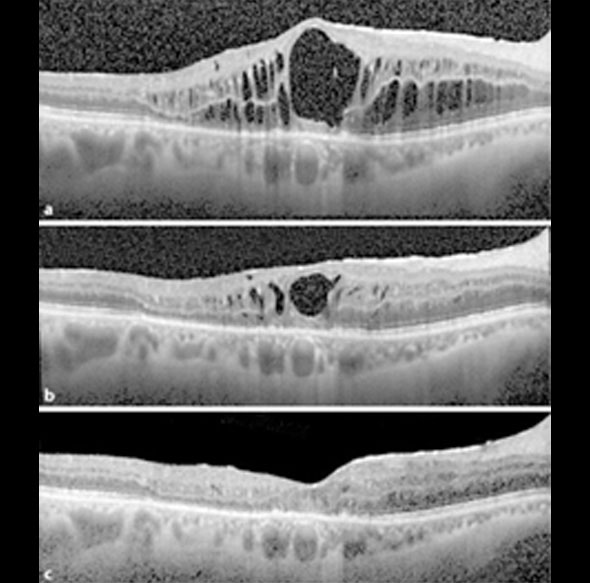
Specialised imaging known as OCT is used in the assessment of retinal vein occlusion